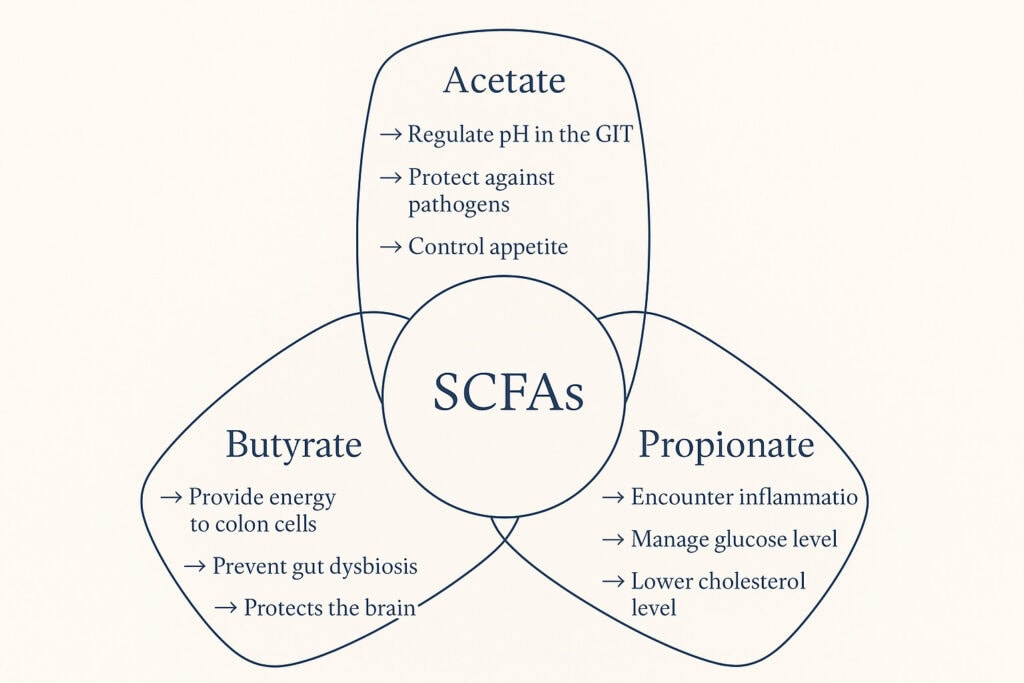
In Part 1, we explored the fundamental role of Short-Chain Fatty Acids (SCFAs) in maintaining a healthy gut microbiome. These powerful byproducts of gut fermentation—produced when beneficial bacteria in your colon ferment resistant dietary fibre—have significant effects beyond the gut, influencing energy levels, managing appetite, and promoting fat burning. A healthy gut microbiome, especially one with high diversity, is essential for optimal metabolic health. In this article, we delve into how these crucial gut metabolites regulate blood sugar, fat metabolism, inflammation, and the renewal of our cellular energy engines: the mitochondria.
SCFAs and Metabolic Hormones: Influencing Appetite and Blood Sugar
SCFAs don’t just stay in the gut; they act as signaling molecules throughout the body. They enter the bloodstream and interact with various tissues, significantly influencing the release of key hormones that regulate appetite, blood sugar, and overall energy balance. SCFAs support glucose homeostasis by improving blood sugar regulation and insulin sensitivity, which can positively impact metabolic health.
The Destination of Energy: Mitochondrial Renewal
While SCFAs act as the messengers, the actual work of energy production happens within your mitochondria—specialized structures inside your cells that convert nutrients into usable power. Emerging research suggests a profound link here: SCFAs like Butyrate don’t just fuel the gut; they trigger “mitochondrial biogenesis.” This is the biological signal for your cells to repair old energy structures and create new, more efficient ones, directly impacting your physical stamina and cognitive clarity.
Uncover Advanced Protocols and Launch Access.
For those who champion evidence over hype.
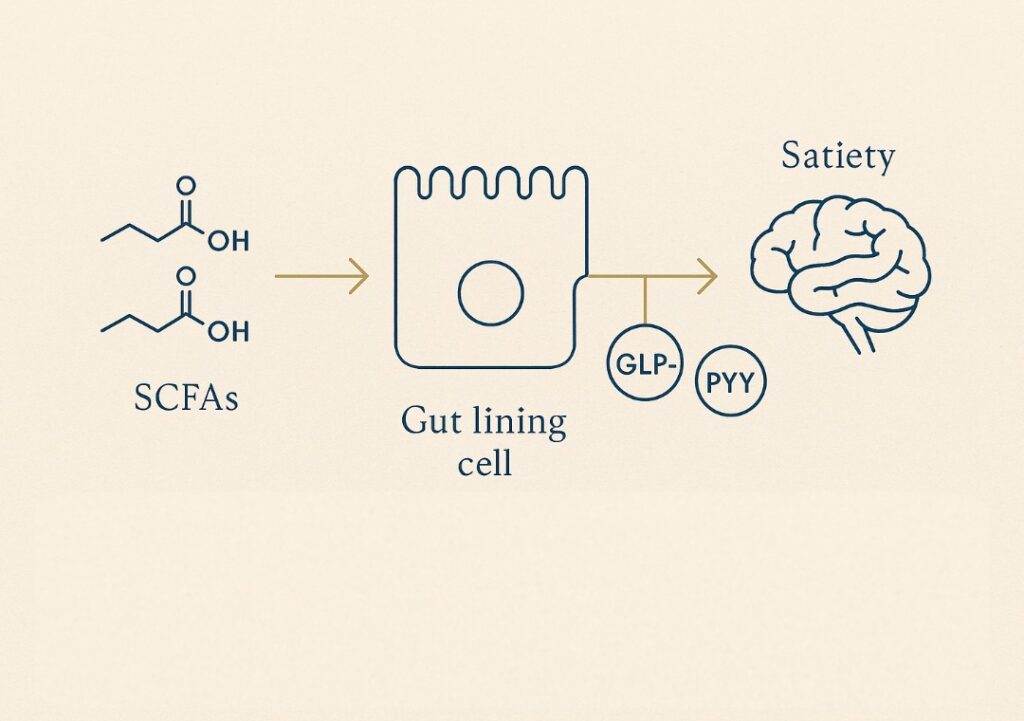
Appetite Regulation via Gut Hormones (GLP-1 & PYY)
SCFAs, particularly butyrate and propionate, stimulate the release of glucagon-like peptide-1 (GLP-1) and peptide YY (PYY), hormones produced in the gut after eating. These hormones signal satiety (fullness) to the brain, helping to regulate food intake. GLP-1 specifically also increases insulin secretion, suppresses glucagon secretion (which raises blood sugar), and slows stomach emptying, further contributing to feelings of fullness. Studies, such as those involving inulin-propionate supplements, show that increasing colonic propionate production significantly boosts GLP-1 and PYY levels, potentially aiding weight management.
SCFAs are also shown to influence body weight regulation, as shifts in gut microbiota and SCFA production correlate with changes in body weight during dietary interventions. You can read more about this in this study: [Frost., 2015]
Enhancing Glucose Metabolism and Insulin Sensitivity
SCFAs, especially propionate, play a crucial role in maintaining stable blood sugar levels. Propionate helps regulate glucose production in the liver. Furthermore, SCFAs can improve insulin sensitivity, meaning your body’s cells respond more effectively to insulin, allowing glucose to enter cells for energy. They do so by communicating with Free Fatty Acid Receptors (FFARs), such as GPR41 and GPR43, which function as sophisticated cellular sensors. These receptors regulate critical internal processes, including the stable management of energy balance and the signalling that dictates satiety, the feeling of being full.
SCFAs can also modulate the expression of genes encoding proteins involved in glucose and lipid metabolism, further supporting healthy metabolic function. This is vital, as impaired insulin sensitivity (insulin resistance) is a key factor in type 2 diabetes and other metabolic disorders. [Zhang et al., 2023].
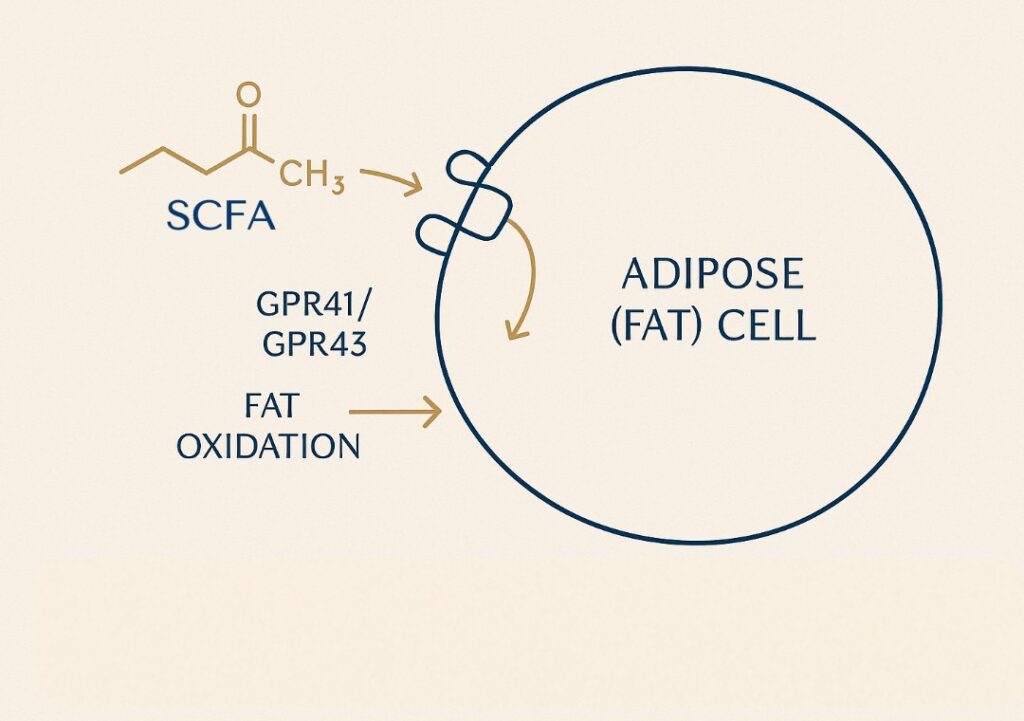
SCFAs and Fat Metabolism: Influencing Fat Storage and Burning
Beyond hormone signaling, emerging research highlights the direct impact of SCFAs on how the body stores and utilizes fat. These gut metabolites interact with pathways that regulate energy expenditure and fat breakdown. SCFAs have been shown to influence fat mass, and their activity is associated with weight loss or prevention of weight gain by modulating host energy metabolism and adiposity.
Promoting Fat Oxidation (Fat Burning)
SCFAs can also play a role in managing how much fat your body stores in its adipose tissue, a scientific name for your body fat. On the surface of your fat cells, there are special “docking stations” or “sensors”—these are known as GPR41 and GPR43. Think of SCFAs as keys that fit into these GPR41 and GPR43 locks. When SCFAs activate these “docking stations,” it’s like they’re sending a message to the fat cell. This message can encourage the cell to start breaking down the fats it has stored and may even help put the brakes on the creation of brand new fat cells. So, by interacting with your fat cells in this way, research suggests SCFAs might help protect against diet-induced obesity. They modulate hunger and metabolism through their effects on gut hormones and lipid metabolism. [Xiong et al., 2022]
Regulating Fat Storage
SCFAs can also play a role in managing how much fat your body stores in its adipose tissue, a scientific name for your body fat.
Think of SCFAs as keys that fit into these GPR41 and GPR43 locks. When SCFAs activate these “docking stations,” it’s like they’re sending a message to the fat cell. This message can encourage the cell to start breaking down the fats it has stored and may even help put the brakes on the creation of brand new fat cells. So, by interacting with your fat cells in this way, research suggests SCFAs might help protect against diet-induced obesity. [Xiong et al., 2022]
Supporting Lipid Metabolism and Cardiovascular Health
SCFAs, particularly acetate and propionate, also influence lipid metabolism more broadly. They can affect cholesterol synthesis and absorption, potentially contributing to healthier blood lipid profiles and reducing cardiovascular risk factors associated with metabolic dysfunction. These changes in lipid metabolism play a significant role in supporting overall host metabolism, impacting energy homeostasis and systemic metabolic health.
Bile Acids: The Overlooked Metabolic Signalling System
Bile acids are not merely detergents for fat—they are dynamic signalling molecules that bridge digestion and systemic metabolism. Synthesised in the liver from cholesterol and stored in the gallbladder, they are released into the small intestine after meals, where they emulsify dietary lipids and facilitate absorption of fat-soluble vitamins. Gut microbes further transform primary bile acids into secondary bile acids via deconjugation, dehydroxylation, epimerisation, and other reactions. These modified bile acids feed back to host receptors that regulate glucose, lipid, and energy homeostasis.
SCFAs help modulate bile acid synthesis, signalling, and recycling, creating a functional feedback loop between fibre-driven metabolism and lipid digestion. When fibre intake is low or the microbiome is perturbed, SCFA production falls, and bile acid metabolism can shift toward more cytotoxic or dysregulated profiles. This shift can impair nutrient absorption, perturb glucose tolerance, and contribute to metabolic risk. Disruption of the bile acid–microbiome circuit is increasingly implicated in metabolic diseases.
Studies in obesity, insulin resistance, nonalcoholic fatty liver disease, and cardiovascular risk show altered bile acid pools and receptor signalling in dysbiosis states. Moreover, bile acids themselves shape the gut community via antimicrobial actions and influence which bacteria thrive.
SCFAs and Inflammation: Impact on Metabolic Health
Chronic low-grade inflammation is increasingly recognized as a key driver of metabolic dysfunction, including insulin resistance and obesity. SCFAs possess potent anti-inflammatory properties that extend beyond the gut, helping to regulate systemic inflammation and support metabolic health. Additionally, SCFAs play a crucial role in enhancing immune function, which not only helps maintain intestinal barrier integrity but also reduces the risk of developing metabolic disease.
Modulating Inflammatory Cytokines
To understand how SCFAs combat inflammation linked to metabolic issues, we need to look at cytokines. Think of cytokines as tiny protein messengers used by your immune system to communicate. Some cytokines act like alarm bells, promoting inflammation to fight infection or injury, while others act to calm things down. Maintaining a healthy balance is key.
Two major players often involved when inflammation becomes problematic are:
- TNF-α (Tumor Necrosis Factor-alpha): This is a primary pro-inflammatory cytokine. It’s often one of the first responders released during an inflammatory event, signaling other immune cells to join the fight. While essential in moderation, chronically elevated TNF-α is linked to various inflammatory conditions, including insulin resistance.
- IL-6 (Interleukin-6): This is another crucial cytokine, often released following TNF-α signals. IL-6 has complex roles – it can be pro-inflammatory, especially in chronic conditions like obesity and type 2 diabetes, contributing to systemic inflammation. However, it also has some anti-inflammatory roles in other contexts. An imbalance, particularly chronic elevation, is linked to metabolic dysfunction.
Research shows that SCFAs, particularly butyrate, can help restore balance by modulating these powerful signals. They can suppress the production and activity of pro-inflammatory cytokines like TNF-α and IL-6, while potentially boosting anti-inflammatory pathways. They achieve this by influencing specific signaling pathways within immune cells and other cell types, helping to prevent the chronic, low-grade inflammation that undermines metabolic health. You can read more about in publication, [Du et al., 2024].
Supporting Immune Balance (Regulatory T Cells)
SCFAs are crucial for the development and function of regulatory T cells (Tregs). These specialized immune cells help maintain immune balance, preventing excessive inflammatory responses and autoimmune reactions. SCFAs also support the health and function of epithelial cells, which are essential for gut immunity and maintaining the intestinal barrier. By promoting Treg function, SCFAs contribute to a less inflammatory internal environment, which is beneficial for metabolic health.
Impact on Muscle Inflammation
An imbalance or deficiency in SCFAs may contribute to increased inflammation in muscle tissue. As SCFAs modulate immune responses, adequate levels may help reduce muscle inflammation associated with conditions like sarcopenia (age-related muscle loss) and support muscle repair and function.
The Gut-Brain Axis: SCFAs Influence Stress, and Cognition
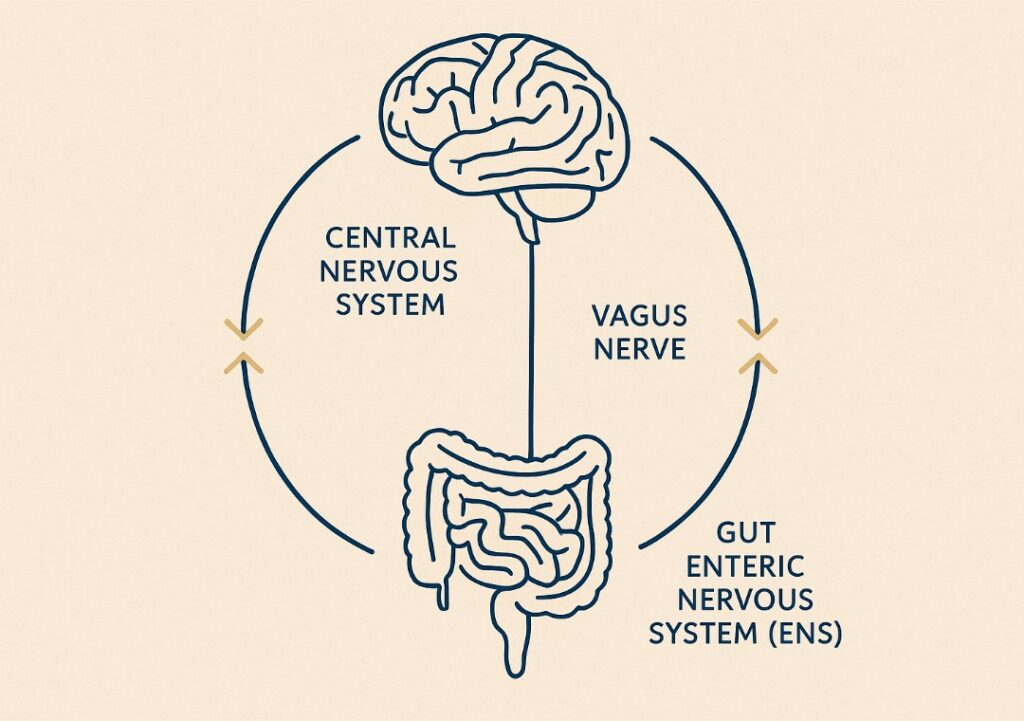
The gut and brain are intricately connected through the gut-brain axis, a complex communication network. SCFAs produced in the gut play a vital role in this communication, influencing neurotransmitter production, stress responses, mood, and cognitive function – all of which can indirectly impact metabolic health. Stress and gut-brain communication can also influence digestive discomfort, contributing to symptoms such as stomach pain, diarrhea, and heartburn.
SCFAs and Neurotransmitter Production
Remarkably, gut bacteria and SCFAs influence the production of key neurotransmitters. For instance, butyrate has been shown to play a role in serotonin synthesis within the gut; approximately 90% of the body’s serotonin (“feel-good” neurotransmitter) is produced there. Balanced SCFA levels thus support stable mood and emotional well-being.
Impact of Mental Health & Stress on SCFAs
The gut-brain connection is bidirectional. Chronic stress, anxiety, and depression can negatively impact gut microbial diversity, reducing the abundance of SCFA-producing bacteria like Faecalibacterium prausnitzii (a key butyrate producer). This reduction in SCFAs can worsen gut barrier dysfunction (“leaky gut,” discussed in Part 1) and inflammation, potentially creating a vicious cycle that impacts both mental and metabolic health. Chronic stress is a major contributor to poor gut health, which can manifest as fatigue, skin issues, and even autoimmune conditions, highlighting the importance of addressing stress to support overall wellbeing. You can learn more about the Gut- Brain axis in our dedicated article.
Modulating Emotion and Cognition
Beyond mood, SCFAs entering the bloodstream can cross the blood-brain barrier or signal via pathways like the vagus nerve to influence brain function, potentially modulating emotion and cognitive processes. Research in this area is rapidly evolving.
SCFAs, Autophagy, and Cellular Health
The metabolic influence of SCFAs extends to fundamental cellular processes like autophagy. Autophagy (meaning “self-eating”), derived from the Greek words for “self” (auto) and “eating” (phagy), is the body’s natural recycling system, removing damaged components and maintaining cellular health, which is crucial for healthy aging and preventing metabolic dysfunction. The plasma membrane plays a key role in mediating cellular responses to SCFAs by serving as the site where signaling pathways are initiated.
SCFAs and Autophagy Stimulation
Research indicates that SCFAs, particularly butyrate, can stimulate autophagy pathways. By promoting this cellular cleanup process, SCFAs help maintain cellular efficiency and resilience, which is vital for preventing the accumulation of damage that contributes to age-related metabolic decline and disease. Enhancing autophagy is increasingly recognized as a key factor in promoting longevity and healthy aging. You can read more about Butyrate production and heath benfits in our dedicated article, What is Butyrate Role for Gut and Overall Health.
The Shield of the Energy Cycle: Redox Balance
As your mitochondria work more efficiently to produce energy, they naturally generate oxidative byproducts (exhaust). To prevent this “exhaust” from damaging the cell, the body employs a protective shield known as the Redox system. The master of this shield is Glutathione—your body’s primary internal antioxidant. By neutralizing cellular stress in real-time, Glutathione ensures the energy cycle remains stable and efficient, protecting the mitochondria from the very energy they produce. You can read more about glutathione in What Are Antioxidants? The Science of Oral Antioxidants for Skin and Overall Health.
The Gut-Metabolism Link to Energy Levels
The profound connection between your gut health, SCFA production, and daily energy is clear. According to current nutrition science, evidence-based dietary strategies—including the use of dietary supplements such as probiotics and prebiotics—can support SCFA production and overall gut health. A well-functioning metabolism, influenced positively by SCFAs and supported by reduced systemic inflammation and a balanced gut-brain axis, is essential for sustained vitality.
Fueling the Body Efficiently
Fueling the Body Efficiently By contributing to stable blood sugar, efficient fat burning, healthy cellular function (via autophagy), reduced inflammation, and potentially a more balanced mood/stress response, SCFAs help ensure your body produces and utilizes energy effectively. Boosting SCFA production through diet is key – see Part 1 for detailed dietary strategies.
The Architecture of Resilience
The profound connection between your gut health, SCFA production, and daily energy is clear. Fuelled by SCFAs, a well-functioning metabolism is supported by reduced systemic inflammation and a balanced gut-brain axis, leading to sustained vitality. By contributing to stable blood sugar, efficient fat burning, healthy cellular function (via autophagy), and a balanced mood/stress response, SCFAs help ensure your body produces and utilises energy effectively.
Ultimately, the insights into SCFAs reinforce the core of Nurture Aging™: true, lasting vitality is cultivated from within. By supporting the communication between your gut metabolites and your mitochondrial engines—and protecting that cycle with internal antioxidants—you honor the inherent design of your biology.

Be first to try our evidence-built formulations.
Collagen Cofactor Complex + Cellular Triad Glutathione Complex.
No noise. No guesswork. Just biologically honest design.
FAQs
Short-chain fatty acids (SCFAs) support metabolic health by influencing appetite hormones (like GLP-1), improving insulin sensitivity and blood sugar control, promoting fat burning, potentially reducing fat storage, and stimulating cellular cleanup (autophagy).
SCFAs help regulate blood sugar by stimulating the release of GLP-1 (which increases insulin), suppressing glucagon, and directly improving how well cells respond to insulin (insulin sensitivity).
SCFAs contribute to weight management by promoting satiety (fullness via GLP-1/PYY), potentially increasing energy expenditure (fat burning), and regulating fat storage. They are part of a holistic approach, not a standalone solution.
The best way is through diet. Focus on eating a variety of foods rich in prebiotic fibers, such as vegetables (onions, garlic, artichokes), fruits (berries, apples, green bananas), legumes, whole grains, and cooked-then-cooled starches (potatoes, rice). See Part 1 [lHow SCFAs Build Your Foundation for Wellness] for more details.